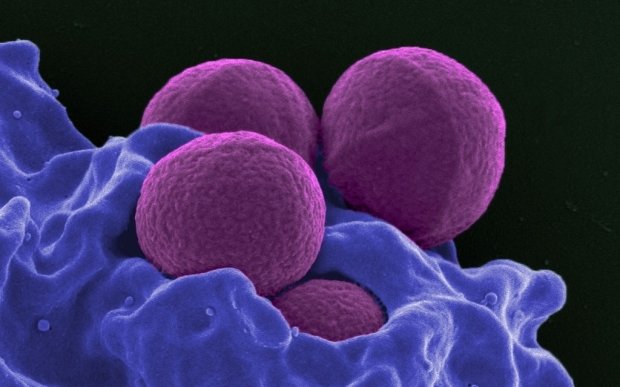
Human neutrophil ingesting MRSA. Image: National Institutes of Health.
You're feeling a bit under the weather so you head to your GP and they diagnose a mild infection and stick you on a two-week course of antibiotics. But after a few days of popping pills you're feeling much better. Do you complete the whole course and finish the prescription?
According to Professor Gwendolyn Gilbert, a Sydney University expert on infectious diseases, there's a very good chance you won't.
In a recent article she wrote for the Australian Medical Journal, Professor Gilbert cited surveys showing that up to half of patients don't use antibiotics as directed. Every official source, from the World Health Organisation to the Centre for Disease Control in the United States to our own Ministry of Health says that's helping to spread antibiotic-resistant disease.
In New Zealand drug resistant bacteria are still rare by international standards but they're becoming more common. Between 2006 and 2008, 2.6 percent of E. coli infections were drug resistant, by 2009-2011 the proportion had risen to 3.8 percent - a 46 percent increase. In 2013 this country saw its first case of a pan-resistant superbug, an infection no antibiotic could cure.
The official advice is that if you don't complete a course of antibiotics then some of the infection-causing bacteria may survive, particularly the ones which were most resilient to the antibiotic.
But in her Australian Medical Journal article Professor Gilbert challenged that argument. "Resistance is much more likely to occur with long antibiotic courses" she wrote. "Premature cessation of antibiotic therapy will not increase the risk that resistance will emerge. For most infections, the recommended duration of therapy (5-14 days, depending on syndrome) is based on expert opinion and convention, rather than solid evidence. However for many syndromes ... there is no difference in outcome when shorter courses are used."
Closer to home, infectious diseases specialist and medical microbiologist Dr Richard Everts has tested the theory out on 42 people suffering from skin infections in Nelson. Dr Everts argued there's mounting evidence that the rules on antibiotic use should be rewritten in some cases.
I'm talking about infections like ear infections, sinus infections, chest infections or maybe skin infections like a boil or cellulitis where it's mild and the antibiotics are working well then we have an increasing amount of evidence that tells us that you can stop your antibiotics when you are feeling substantially better, rather than continuing to the end of the full course.
Both Dr Everts and Professor Gilbert agreed that long courses of antibiotics are still needed for serious diseases like tuberculosis and for infections in hard to reach places like bones or inside an abscess.
Dr Mark Jones, an infectious disease specialist at Wellington Hospital and Aotea Pathology, said that while there is strong evidence that stopping antibiotics early can help fight microbial resistance without compromising recovery, it's not a decision patients should be making on their own.
"I think they should negotiate that with their GP or their doctor at the time they are prescribed and the doctor should either say 'you must complete this course' or 'if you're feeling better you can probably stop taking them at such and such a stage.'" Dr Jones said.
The New Zealand Royal College of General Practitioners says it is not common practice for GPs to tell patients to stop taking their course of antibiotics once they feel well. It says patients will only normally be told to stop taking antibiotics early if they suffer side-effects or tests prove they don't need the drugs.
Links:
- "Knowing when to stop antibiotic therapy" by Professor Gwedolyn Gilbert
- Advice on antimicrobial resistance from the World Health Organisation
- Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data (pdf)
- Rising antimicrobial resistance: a strong reason to reduce excessive antimicrobial consumption in New Zealand

