Pharmac is ditching a policy that required New Zealanders diagnosed with HIV to reach a threshold of illness before receiving treatment.
Photo: 123RF
The approach, which deprived New Zealanders diagnosed with HIV of immediate treatment, is being revoked, two years after Pharmac received clinical advice that a change would be in the public's best interest (PDF, 47.8MB).
The long-standing policy stated that those diagnosed with HIV had to wait until their immune system had been damaged before they could start therapy, only receiving medication when their immune cell count was well below the average.
Pharmac spokesperson Sarah Fitt said the change in policy only became possible with the lift in the Combined Pharmaceutical Budget announced in May.
The change is set to take place on 1 July, and comes after a petition calling for an end of the restrictions was signed by 5709 people.
New Zealand AIDS Foundation (NZAF) executive director Jason Myers said the petition was launched "because we wanted to add some public pressure given it had been so long since Pharmac had received advice to change the threshold, but it hadn't happened".
NZAF organised the petition on their website between October and May.
"We cannot directly attribute the petition to the change in policy," said Mr Myers. "Pharmac have a number of very sophisticated criteria that they use to decide whether or not to fund particular medicines. In fact, public pressure is not one of them."
Mark Fisher, executive director of HIV advocacy group Body Positive Inc, said there were a number of people who did not have access to treatment at time of diagnosis, due to the restrictions that were in place until now.
"We had one person who had to wait four years before being provided with their medication, not able to access treatment until then, even though he wanted to start therapy," said Mr Fisher.
Body Positive Inc advocates on behalf of HIV+ people, and was founded by - and run for - people with HIV/AIDS.
"With the advancement in treatment we should not have any AIDS diagnoses," said Mr Fisher.
"Removing the CD4 threshold [immune cell minimum requirement] will help."
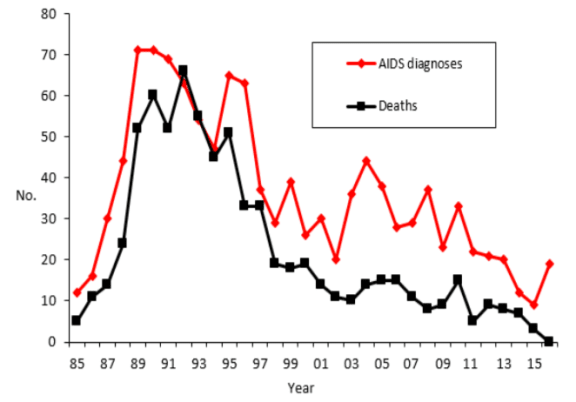
Annual number of diagnoses of AIDS and deaths among people notified with AIDS. Graph / NZ Aids Foundation Photo: Supplied
In 2016 there was a 156 percent increase in the number of AIDS diagnoses in NZ, and 16 of those were diagnosed within three months of their HIV diagnoses.
Overall 23 people - 20 men and three women - were diagnosed with AIDS in 2016, compared to nine people in 2015.
There were a record number of new HIV cases in 2016, with 244 people diagnosed in 2016, up 20 from the previous year.
Louise Bourchier, sex educator and lecturer in health promotion at Unitec, agreed that the restrictions needed to change.
"Some medication simply isn't available here. The medication that is [available], requires a minimum level of sickness," said Ms Bourchier.
"If someone healthy was diagnosed with HIV, they would have their treatment delayed until they got sicker.
"This was a problem because when people were getting sicker, it was doing lasting damage to their body."
Mr Fisher concluded that the sooner people had access, the better.
"Once people are engaged in care, they can be given medication that allows them to sustain an undetectable viral load. This means they cannot pass on HIV to their sexual partner.
"It's a win-win situation in which the person lives a healthy life and doesn't transmit HIV."
Pharmac spends about $35 million a year on 21 HIV treatments, which were accessed by about 2500 New Zealanders.


