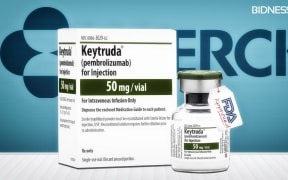
A woman ill with melanoma has some big questions she wants answered before she will consider bailing on Keytruda, and opting for a soon-to-be Pharmac-funded alternative

Photo: 123rf.com
The drug-buying agency yesterday announced it will fund the immunotherapy drug, Opdivo, for 350 patients with advanced melanoma, from July.
Joy Cole, 71, has made the road trip from Porirua to Auckland with her husband, Geoff, 70, three times so far for treatment.
Mr Cole said his wife was already part way through the treatment, they did not know what the side effects of Opdivo were and whether she could switch from Keytruda to it.
"Opdivo doesn't become funded until the 1st of July, so Joy has probably two or three more treatments to go before the 1st of July.
"Before we really need to make a huge decision on the dollars, it's going to be early or mid-August. So hopefully by that time we'll know from the oncologists and the specialists what the deal is between Opdivo and Keytruda.
"If all the signs say that Opdivo is going to do the same or better, then we'll switch."
Mrs Cole said there was some concern about the funding only covering up to 12 weeks of treatment.
Mr Cole said the question was over what happened at the end of that period if more was needed.
"We don't know whether or not six infusions of Opdivo are sufficient. What happens if people need, I don't know, 20 infusions but only six of them are funded.
"Who picks up the tab for the other 14?"
He said the plan was for Mrs Cole to have at least one more Keytruda treatment, followed by a CT scan to see if it was working, before they decided whether to switch to Opdivo.
'Everyone else out there now can get cured'
Meanwhile, a woman who has lost six friends in the past three years alone to Hepatitis C, is overjoyed that the drug which cured her will be fully funded by Pharmac.
Yesterday, the drug-buying agency announced it will fund Harvoni and Viekira Pak - both of which are proven to have a more than a 90 percent success rate after 12 weeks of treatment.
Rachel Stace said when she contracted Hepatitis C about 10 years ago, it was a possible death sentence.
But she said that all changed a few years ago, when she was put onto a 12-week trial of Viekira Pak by Auckland City Hospital liver specialist Dr Edward Gane.
"And it cured me. There were a few side effects but nothing, nothing like the [other cancer drug] Interferon.
"A friend of mine did it with me, she had the same result. We both ended up cured, when we thought it would never happen, after 12 weeks.
"And since then, Ed has gone on to put several of my friends, who thought basically they were facing a death sentence, [on it]... He's put them on other drug trials and they've been cured as well."
She said they were all extremely grateful to get a second chance at life.
Ms Stace said it was amazing that the drug that cured her will now be funded.
"It just makes me sad that my friends didn't have to die. But it means that everyone else out there now can get cured.
"They don't have to pay for the treatment, it doesn't matter where they are in New Zealand, they don't have to be in Auckland for a trial. They can be cured."
Pharmac said the cost of Viekira Pak was about $49,000 for a 12-week course and would benefit the 11,500 people with chronic Hepatitis C, while Harvoni will help 250 people with severe liver disease at a cost of about $73,000 per patient.
A liver specialist said Pharmac's decision to open consultations on treatments for Hepatitis C was a huge advance for those living with the disease.
A liver specialist at Auckland City Hospital, Ed Gane, said the new oral medicine, taken over 12 weeks, has far fewer side effects than those previously available.
"Up until now, the treatments that we have had have been poorly tolerated. People need to take a year of weekly injections, often associated with debilitating side effects, and the number of people who finish treatment is significantly lower and the cure rates are less than 50 percent."
Political reaction
Pharmac said up to 700 patients with advanced melanoma could be treated with the new publicly-funded drug this year.
Pharmac still needed to consult clinicians and the public over the move, but Opdivo could be funded from July.
Chief executive Steffan Crausaz told Morning Report the drug will treat about a 350 patients a year, but almost double that in the first year.
He said the process had been fast-moving.
"Opdivo has only been available for supply in New Zealand since last week, when it got approved by MedSafe, the regulator of medicines in New Zealand. So the processes acted very promptly in terms of that treatment."
But opposition political parties are demanding details on the plan for the $50 million cash injection into Pharmac .
The Green Party is demanding proof Pharmac would have the money it needed to fund the new medicines.
Greens health spokesperson Kevin Hague said the agency was already under-funded and it was not clear if the extra money was enough.
"New Zealanders need to [know] hat Pharmac was recommending was necessary in order to not only keep parity with the level of access of drugs that New Zealanders already have, but then to extend that sensibly."
The Labour Party said the plan was a rushed attempt to dampen the controversy over funding for a drug for advanced melanoma.
Health spokesperson Annette King said the government should be giving Pharmac more money.
She said it only had enough for seven new drugs and not enough for the 20 it wanted to fund.
The Cancer Society said Pharmac's plan to fund a new medicine for people with advanced melanoma fell short, and would not help those who need treatment now.
Opdivo could be funded from July, but the Cancer Society's medical director Chris Jackson said some people with the cancer did not have that sort of time to wait.
He said it was time Pharmac took a different approach.
"We favour an access-to-medicine scheme, whereby truly breakthrough drugs in areas with high un-met need and no effective options available, that patients will have temporary access while Pharmac does what it does best, which is get best possible value for money. But in the meantime, people are missing out, and people are suffering."