The public health system is over-stretched and some people need help to get answers to serious problems more quickly, a Whakatāne surgeon says.

Photo: 123RF
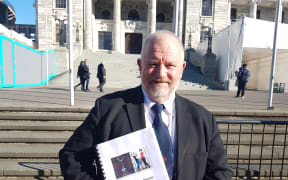
Surgeon Paul Anderson and others set up the Emergency Assessment Fund (EAF) early this year to provide what he described as an "innovative response" to delays.
Those delays were being cause by the contentious non-urgent or elective health system, under which only those patients who are considered urgent enough and who can be seen within four months are accepted.
It led to thousands being declined amid ongoing claims about so-called "unmet need".

Whakatāne-based surgeon Paul Anderson Photo: Supplied
Dr Anderson said the EAF had a free specialist assessment clinic attached to it, which he runs weekly at the Ōhope Beach Medical Centre.
He said there was a two to three-week waiting list, but it could see patients and fund those considered urgent enough who lack the ability to pay to see a medical specialist privately, and for some tests.
Patients could get a diagnosis rapidly and find themseves higher up the priority list in the public system as a result, he said.
"And usually what happens is that all those specialists are attached to a [public] hospital.
"So if they see that patient and decide there is genuinely an urgent problem that needs to be done, they then can feed them into the hospital with an urgent rating."
A 67-year-old Bay of Plenty woman who wishes to be known only as Kathleen said she has had a heart murmur all her life. She had been told it was "nothing", but it worsened.
After a two-year wait she was seen at Whakatāne Hospital but was unhappy with the care she received. The cardiologist "was a youngish chap who was quite flippant about my heart problem, which is quite serious".
She said it "frightened the living daylights out of me" not to understand what her problem was or having it explained.
She got $350 from the fund to see another heart specialist privately.
"This guy was terrific. He explained it all to me, I understand it, he told me at this stage there was nothing to panic about but it was going to get worse and I would have to have surgery. Well, you can cope with that."
Dr Anderson said he'd seen between 130 and 150 patients through the clinic and up to 40 had received funding for a specialist assessment and intervention.
" general surgeon's just helped us out with an ongoing patient that had had chronic pain for approximately five years. Everyone was concerned about it and we found out that it was due to a mesh he's had implanted. And then as a result of that assessment he went in as an urgent case to have that mesh removed and he's now got his life back."
Dr Anderson said the public health system was excellent, just overloaded in terms of resources.
"Or under-resourced and probably not enough specialists. And just through the free clinic that I run ... there were patients coming through that were having to wait seven or eight months, whether it's for something like an echocardiogram or an ultrasound or a CT scan, to even then get to see the specialists, and some of them quite concerned [and] didn't have enough money to go privately."
A Bay of Plenty District Health Board spokesperson said it was not aware of the EAF and staff were not involved in it. There had been significant improvements in waiting times for elective surgery at the DHB over the past five years, they said.
A total 11,315 people in the district had their elective surgery at public hospitals in the last 11 months, which was 703 above the government target for last year, the DHB said.