In our conversations about mental health, whose stories are told the loudest? A contributor writes why those with first-hand experience of mental illness should be able to define their own narratives.
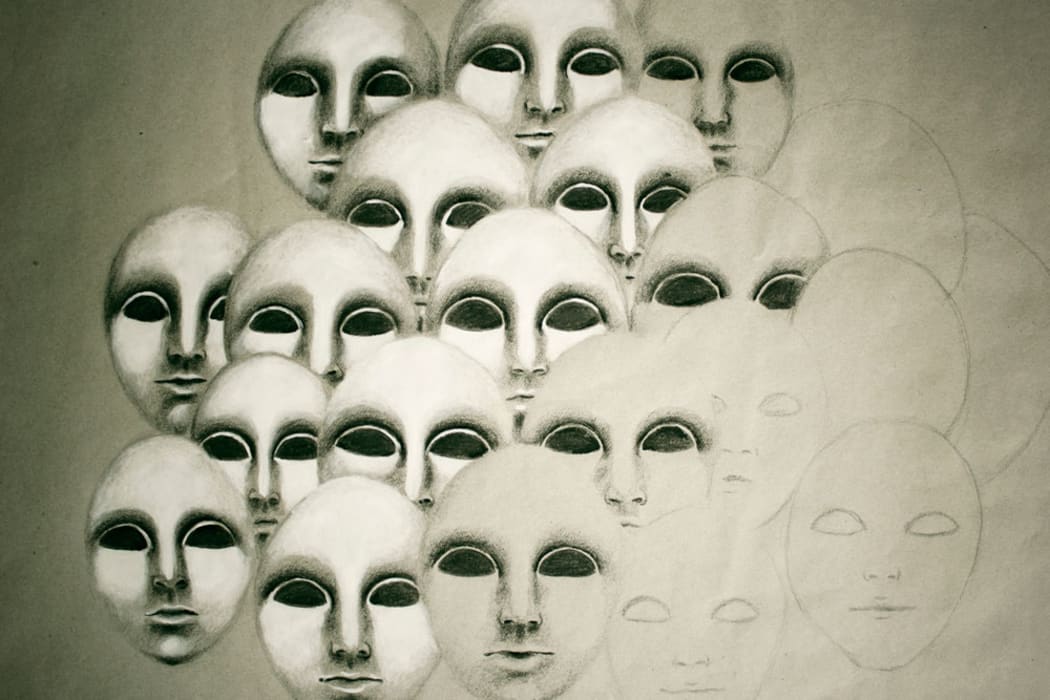
Photo: Image: 123RF
Here’s something you can try at home: input ‘experience with depression’ or ‘experience with anxiety’ into Google. You’ll yield a plethora of first-person essays and experiential accounts, many of them quite good. But substitute ‘depression’ for, say, ‘manic bipolar,’ ‘schizophrenia’ or ‘psychosis’ and you’ll notice at once the dearth of pieces written by sufferers of the conditions. Instead, medical discourse speaks on their behalf; their lives are rendered in symptoms, manifestations, peculiarities, statistics, jargon, discussions of Types (I, II, III…).
Failing that, you’ll get dramatic first-person accounts from family members and loved ones of the afflicted; stories from people who had to watch someone they care about succumb to irregular brain chemistry.
Want to read more? Browse the rest of our mental health coverage here.
It’s not coincidental that the divide between, say, depression and disorders like schizophrenia are demarcated by the threshold between sanity and its opposite. Madness means having the ability to speak for yourself stripped from you, or have your narrative focalised through other lenses.
This is not a flash in the pan. This is the deliberate backgrounding of people in favour of dominant medical and societal structures. This is a problem.
***
In a way, it was heartening to see a recent depression ad campaign featuring a sufferer who wasn’t white. Maori and Pasifika people, especially young and male, top the list of both suicide demographics and the list of those who lack access to adequate mental health support.
This is not a flash in the pan. This is the deliberate backgrounding of people in favour of dominant medical and societal structures. This is a problem.
However, the sufferer doesn’t speak about his illness first-hand – the role of narrator is given to an outrageously adorable young family member. He is seen enjoying himself, partaking in a wee spot of our nation’s favourite pastime: Rugby. He is presented as happy. There are reasons for this, perhaps sound. Sometimes this narrative of hope – that you can and will get better – is all people have to cling onto, their only glimmer of light. More cynically, showing someone crying in bed, physically unable to remove themselves because of the practically tangible crushing weight that sits atop their chest every second of every day – well, that would be a bit downbuzz. Or, to put it another way, it wouldn’t be palatable.
***
Similarly parochial was a recent campaign which encouraged people to write on their hands in support of people suffering from depression. It struck me as odd that the hands and wrists, the focal site of many expressions of self-harm, were unblemished in all the photos. There are expedient reasons for this perhaps – fear of copycatism, or susceptible teenagers following suit – but the lack of these physical manifestations of many people’s mental illness made the campaign feel strangely neutered and tokenistic. It’s all very well to make gestures -- but if they don’t include and target the people they’re trying to help, those gestures end up empty.
***
It is this desire to elide from the horrors of mental illness, to bleach it of all the factors that might disquiet people, that makes campaigns like these such failures.
The dominant narrative of hope and, indeed, cure is disingenuous. As anyone with a mental illness can tell you, emphasis is not on complete remedies but on strategies for coping. The effects of this on sufferers, once this false narrative is ripped away, can be catastrophic: what happens when there is no light at the end of the tunnel?
***
For me, I think of my mania as a time inhabiting a headspace where traditional conceptions of sign and referent, signifier and signified become tangled and confused. I don’t think of it as madness per se; just perceiving the surrounding world in a different way, with a different set of compulsions and structures. Imagine being really starving - ravenous - but instead of needing food you need to catch a certain bus to sustain you. Or imagine a world where every action, even if it seems unrelated, can be connected synchronically, and every one of these connections has a sort of meaning to it that’s just beyond your grasp but if you just stretch out, just a little more --
It is this desire to elide from the horrors of mental illness, to bleach it of all the factors that might disquiet people, that makes campaigns like these such failures.
So it’s a bit bizarre and scary, but I don’t think it’s useful to talk about it in terms of unreality or madness -- instead, think of differences of perception. It’s not as though I get invested one hundred percent, although sometimes my brain feels a bit like it’s disintegrating somehow. It’s like having the trickle of street noise you can always hear in the background amped up to 11, torrents of water pouring in and sinking the ship. Or less fatalistically? Just a different way of seeing the world for a given period of time.
***
The most basic rule of narrative is the distinction between sympathy and empathy, or between understanding and identification. If you’re trying to get undiagnosed sufferers to come forward, you need to offer a story or trajectory that they can identify with, which is why white-washed depictions of mental illness can discourage people from coming forward for fear that what they have is much, much worse, or that their illness doesn’t look anything like that.
This is especially true if narratives don’t even bother to target them; while illnesses like schizophrenia or agoraphobia get ecumenical nods in any discussion of mental illness, there aren’t any first person resources they can comb, no solace they can reap in the words of others.
For non-sufferers, mental illness is presented as something that it isn’t. Most presentations are illusory. How can they understand or know what to do or what is needed for people who suffer mental health if they’re getting a stunted picture of what it looks like?
And what of the conditions that are perceived as synonymous with, or at least conducive to, madness; what voice are they allowed? The descriptor of ‘madness’ robs them not just of dignity but of the human right to expression.
Some might argue that the people mental health discourse marginalizes are incapable of coherent communication. But people will always be attracted to stories that resonate with them personally. In denying the ‘mad’ their story, even if not conventionally formulated or structured we’re forcing other mental illness sufferers into the dark. It’s an irony that the people whose voices we need to hear from most in the campaign find it difficult to discover an outlet for their voice. We are so used to other people speaking for them that their own voices will be, at first, distant and alien.
To have a condition that renders you ‘mad’ in the eyes of society and medicine is to have your vocal chords excised, your hands amputated, expressions sedated.
This current state is bolstered by the way we deal with all mental illness, narratives that purge it of its unsavoury aspects and transmute it into a bit of gloom - an assertion that couldn’t be further from the truth of the illness.
Until a depression campaign features someone talking about the cuts on their wrists, or until stories from family members of those diagnosed with more severe mental illness’ don’t dominate but compliment - or better, supplement - general discussion, our views of mental illness with continue to be myopic and half-formed. Those who need help the most will continue to suffer.
This author has chosen to remain anonymous due to concerns about stigma surrounding mental health.
To find more stories on mental health, click here.
If you need to talk to someone about your own mental health, try these helplines. If it is an emergency, call 111.
Lifeline - 0800 543 354
Depression Helpline - 0800 111 757
Healthline - 0800 611 116
Suicide Crisis Helpline (aimed at those in distress, or those who are concerned about the wellbeing of someone else) - 0508 828 865 (0508 TAUTOKO)
Youthline - 0800 376 633, free text 234 or email talk@youthline.co.nz

