Mike Berridge on the effects of our microbial friends on gut inflammation, immune disorders and maybe even our mood.
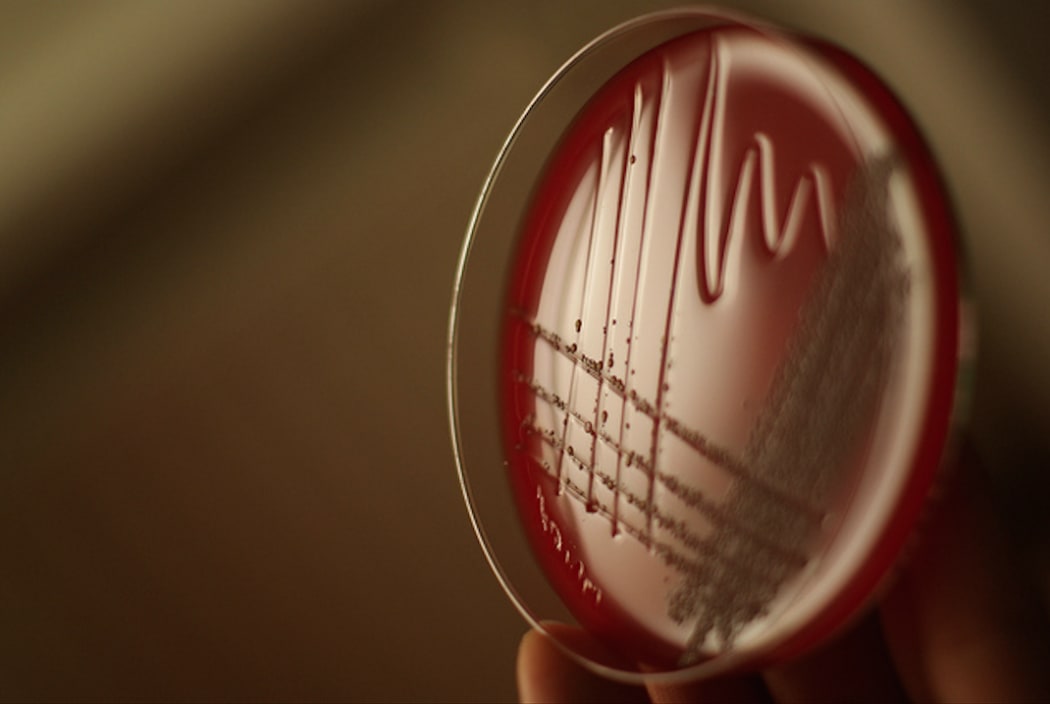
Photo: Petra B. Fritz / Flickr
Microbial life gave rise to complex organisms several billion years ago. Today 70 percent of the biosphere is microbial. Consequently, all complex organisms exist in a sea of microbes that coat the surfaces of the body, populate the digestive tract and line the lungs. Our microbial partners equate to the number of cells in the human body, the vast majority residing in the colon. Breaching the skin barrier or internal linings of the body results in acute infection that can rapidly overwhelm the immune defences of the body.
A well-balanced microbial flora often referred to as our microbiome is essential for good health and contributes to digestion. When this balance is disturbed, for example with poor diet or with broad spectrum antibiotics, a cascade of events results that can include inflammation and inappropriate activation of the immune system, and this can lead to chronic and sometimes acute health consequences. For example, a serious gut infection results when the bacterium Clostridium difficile establishes itself in the colon resulting in a type of colitis. In cases where these organisms do not respond to antibiotics, faecal microbial transplantation is now recognised as a treatment of choice in some countries, being 85-90% effective with a single treatment in most patients. This rebalances the microbial content of the gut, sometimes with non-pathogenic strains of the same bacterium.
The use of gut microbes to treat intestinal disease has a long history dating back thousands of years. Then in the second half of the nineteenth century, germs were found to cause infectious diseases. The subsequent discovery of antibiotics revolutionized the treatment of these diseases saving millions of lives. However, the overuse of antibiotics and excessive hygiene has generated a new set of health problems that we are only now beginning to fully comprehend. Broad spectrum antibiotics not only kill the problem microorganism but also destroy many of the beneficial bacteria, including gut microbes that contribute to digestion and maintain gut health.
While faecal transplantation is becoming more widely accepted for some forms of colitis and other inflammatory bowel diseases, and alternative methods of colonic microbe rebalancing are being introduced, the application of faecal transplantation to autoimmune diseases not directly affecting the gut, to metabolic syndrome that leads to diabetes and cardiovascular disease, and to mood modification and neuropsychological disorders are less clear.
READ MORE: I've had four faecal transplants.
Because our microbiome is inherently part of our human being, we can consider ourselves a walking ecosystem from birth to death with a significant amount of the control of that ecosystem being in our own hands. Dietary intervention is perhaps the simplest and most accessible place to start following first line medical advice, or better still, alongside medical approaches. Following World Health Organization and Ministry of Health dietary advice of increasing fresh fruit and vegetables, reducing foods with added sugar and rebalancing fat and oil intake away from pro-inflammatory omega-6 polyunsaturated fatty acids towards omega-3 in fish and some vegetable oils, and omega-9 in olive oil and avocados is a good place to start. Prebiotics and probiotics can help some individuals and identifying food intolerances such as gluten and dairy products is important. Persistent disease symptoms warrant further exploration, and this is where faecal microbiota transplantation is an option. Treatments that alter our microbiome are much more acceptable and effective than they were 5 years ago, although here in New Zealand the practice is not particularly common and the procedure tends to fly under the clinical practice radar.
While there is a direct link between our microbiome and inflammatory bowel conditions like Crohn's disease, ulcerative colitis and irritable bowel syndrome, the links between microbiome quality and autoimmune diseases like ankylosing spondylitis, Sjögren's disease, various forms of arthritis and multiple sclerosis are more difficult to understand. Nevertheless, outcomes can be life-changing. Factors that affect response include individual tissue type (e.g. HLA-B27 is a known risk factor for ankylosing spondylitis), subclinical gut inflammation, immune cell activation and molecular mimicry that fires up seemingly unlinked immune responses. However, in most cases, the combination of factors contributing to these diseases are poorly understood.
Another area of intense investigation is the relationship between microbiome and mood. Certain microbes in the gut produce short chain fatty acids like acetate, butyrate and propionate and precursors of serotonin (regulates anxiety and depression) and dopamine (feel good hormone) which are major regulators of brain function. Although there is some debate about whether the serotonin produced in the gut is active in the brain, the second largest collection of neural cells in the body is around the gut with links to the brain via the vagus nerve.
While our germ phobia has largely been focussed on bacteria, other microorganisms such as fungi, archaea and some parasites are also important contributors to our microbiome. Imbalance in any of these microbes can potentially contribute to disease. Manipulating our microbiota for better health is now moving into mainstream medicine as a realistic option when other options have been exhausted, but because lifestyle and dietary changes can play a major role in gut health and inflammatory diseases, these approaches should be considered alongside faecal microbiota transplantation procedures.

