Professor George Jelinek was 45 and at the peak of a distinguished medical career, when he was diagnosed with multiple sclerosis (MS) - the disease which had destroyed his mother's life.
He set his mind to tackling the issue at the roots and eventually developed a programme for people with MS, which he documents in his Overcoming Multiple Sclerosis Handbook that has just had a third update republish.
Twenty-three years later, prof Jelinek is symptom free, and is the founder of the Neuroepidemiology Unit within the Melbourne School of Population and Global Health at The University of Melbourne.
Photo: supplied
MS is a neurodegenerative disease that mainly affects the brain and spinal cord, often coming in midlife or even in young adults, and in many cases leading to profound disability, prof Jelinek says.
But even those that don’t progress to that level can still develop significant problems such as cognitive disability and a variety of symptoms that most can’t see like bowel and bladder disturbance or immense fatigue, he says.
At the time of his own diagnosis, he was at the helm of his career - a professor of emergency medicine and editor-in-chief of a major medical journal.
“Seeing what happened to my mother, she was diagnosed at pretty much the same age as me, at around 45, and then, less than a decade really, at my graduation from medical school, for example, she turned up in a wheelchair,” prof Jelinek tells Kathryn Ryan.
“Within a few years from that, she was essentially bed-bound and really could no longer feed herself and we had to help her with all her sort of normal bodily functions and daily activities and she ultimately took her own life.
“Then 18 years later, to be sitting in the neurologist’s office and to have the neurologist talking to me about MS in sort of general terms, when I’d gone to see him with a numb leg and backside, I was in such profound denial that I actually couldn’t even relate what he was saying to me, until he eventually had to be much more direct and said ‘look you’ve got MS’.”
At first, he felt his world fall apart and couldn’t see any way out, he says, until some good friends and colleagues guided him on how he could manage his illness.
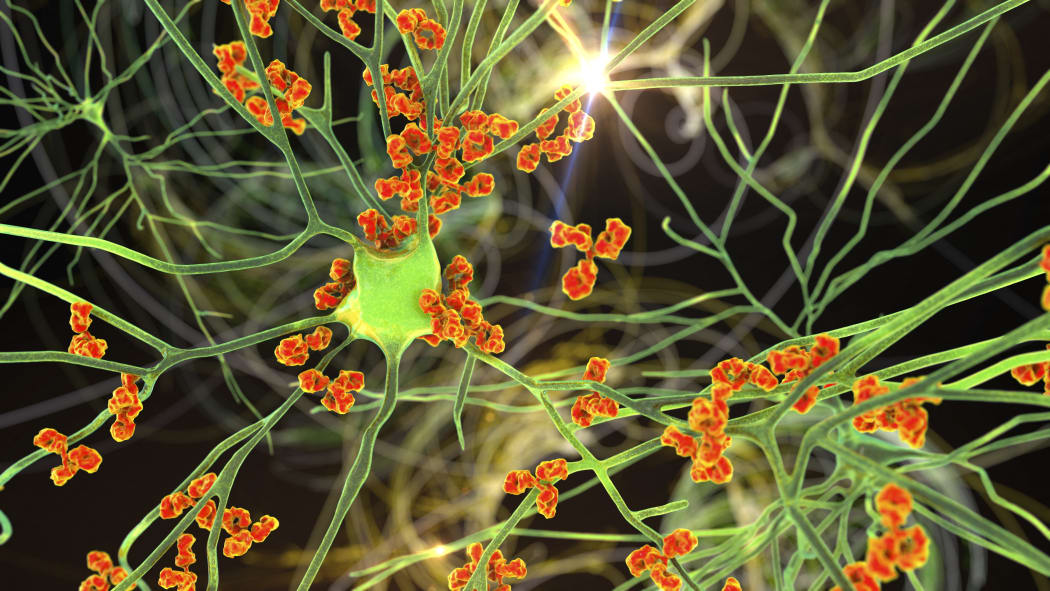
In cases of MS, the body’s own immune system attacks the central nervous system, which causes communication problems between the brain and the rest of the body. (Illustration image) Photo: KATERYNA KON/ Science Photo Library via AFP
So, after learning everything he could about MS to prevent his life deteriorating, he devised the Overcoming Multiple Sclerosis Programme which looks at diet - cutting out dairy and meat, and reducing fat intake - exercise, vitamin D, and Omega 3.
“Typically, these are things that affect the immune system so people who eat a diet that’s heavy in animal fat and dairy, people who don’t get much sunshine, particularly in childhood, and one of the really key things that’s coming out now is infection with the glandular fever virus, Epstein-Barr virus.
“There’s a number of other factors like smoking and stress that typically exacerbate that risk [of MS] to the point where if you have all those operating and you have that genetic susceptibility then there’s this cascade of events that results in immune attack by the body’s own immune system on your own central nervous system.
“When the immune system does attack, the brain sets up an inflammatory response.”
Some use immunosuppressants to try and dampen down that inflammatory response, but prof Jelinek says his approach is about doing that in a natural way through lifestyle changes.
“One of the things that’s probably not widely understood is that the white cells of the body … are responsible for driving this immune inflammatory response.
“The white cells secrete chemicals that do that and the things that makes these chemicals are actually ingested in the diet. Typically, these are fats, fatty acids, so that if we have a diet that’s rich in animal fat and Omega 6 fatty acids, which typically we get in a range of different vegetable products … tend to promote inflammation.
“Whereas the Omega 3s, which I think most people have heard of now, which we get in fish but also in plant sources like flaxseed and flaxseed oils but also walnuts and pecans and a few other sources, they tend to dampen down this inflammatory response.
“Now we need both Omega 6s and Omega 3s, but they have to be in right sort of ratio to get that optimal immune balance. Typically, that’s a ratio of about two Omega 6s to one Omega 3 and typically Western diet at the moment has a ratio of about 25 to one rather than two to one.
“So, changing the oil composition of the diet actually naturally resets the immune system towards an anti-inflammatory setting.”

Finding the right ratio of Omega 6 and Omega 3 food sources (pictured) can help better manage cases of MS, says professor George Jelinek. Photo: 123RF
Researchers found those living further away from the equator – and therefore less exposed to the sun - were more likely to have MS as well as more profound cases of it, he says.
“But vitamin D is only part of the story, it seems that the sun acts on your skin to directly affect a lot of the immune cells that live just under the skin as well as creating more vitamin D in the body and vitamin D we know is … profoundly anti-inflammatory, it’s also quite neuro-protective.
“So, we, sadly, in New Zealand and southern Australia have a real issue with vitamin D deficiency. In Australia, around about 70 or 80 percent of people in Melbourne for example are frankly deficient in vitamin D throughout winter.”
Those who are depressed also have more inflammatory chemicals and that makes it worse for those with MS.
“Depression, which is as you say can be easily seen as a result of having the illness, but unlike most other autoimmune diseases, it’s got a very high incidence in MS so about one in every two people with MS will become depressed at some point during the illness. With most other autoimmune diseases, it’s a far, far lower proportion than that.”

The winter blues is a real phenomenon based on low vitamin D, which can be attained through sunlight exposure, says professor George Jelinek. Photo: 123rf.com
Prof Jelinek has done such a good job of managing his illness through his lifestyle changes that some now question if he ever really was diagnosed.
Fifty people have contributed to his handbook which includes health professionals discussing how they adopted the MS programme.
“It’s no longer about whether or not I have the diagnosis and those sorts of things. Here are 50 odd people who are living this programme, have had extraordinary results, and we’ve collated all their advice and wisdom into one book for people to read.”
Although, he says, many health professionals somewhat still discount diet within treatment of MS.
“I have to say a lot of the work we’ve done at the Neuroepidemiology Unit has been on a very large cohort of about 2500 people with MS worldwide and we’ve tracked them now for seven and a half years and looked at how their baseline diet and how they’ve changed their diet over the years has affected their course.
“To nobody’s surprise really … there’s a very significant association between high quality diet and better outcomes over time, over that seven-and-a-half-year period.
“And wherever it’s been studied essentially, there’s been quite dramatic effect of diet particularly omitting animal fat as much as possible, on the course of MS. It’s difficult when you scan the literature to find a paper, but dozens support this.”

